Benign Ovarian Tumors Pdf
Posted By admin On 31.08.19Despite the heterogeneity of ovarian tumours, trisomy 12 is frequently found in the different subtypes of borderline and benign ovarian tumours of germ cell and sex cord-stromal origin, suggesting a common pathogenesis, at least for the initial stages of tumourigenesis.
Windows software licensing tool. To obtain and run the Software Licensing System Reset Tool, follow these steps: Click the Download the Software Licensing System Reset Tool package now link to start the download. When you receive the File Download dialog box, click Desktop then click Save. The other one that seems to be related to error 1628 is error 1722 (problem with the Installer Package). The KB928080 is the fix for that one. Here's the link if you wish to try this one: This is the Software Licensing System Reset Tool Package. Even though the. Received error message when I downloaded Software Licensing Reset Tool for error message 1722 on FSX From the other thread. Error message 1722 and 1605 when reinstalling. Download System rest Tool and it gives me an Error message also. I have the same question (27).
Benign Ovarian Tumor Symptoms
- Ovarian cancer among women with benign ovarian tumors and biolog-ical mechanisms involved in the transformation of benign ovarian tu-mors to ovarian cancers have been proposed 11–13.Inaddition,it has also been suggested that borderline ovarian tumors may evolve from benign ovariantumors 11, but to ourknowledge, only two stud.
- Diet and benign ovarian tumors (United States) Results: The risk of BOTs was elevated for the highest vs. Lowest quartile of intake of total, vegetable, saturated, monounsaturated, and polyunsaturated fat. The corresponding age-, hospital-, total energy-, and body mass index-adjusted odds ratios (ORs) and 95% confidence intervals (CIs).
No notes for slide. If ovulation does not occur, a clear fluid filled follicular cyst lined by granulosa cell may result. Notice the smooth inner lining of this cyst, which is nothing more than a follicle which has gotten large but neither burst nor undergone atresia. When ovulation occurs, corpus luteum is formed that may become abnormally enlarged through internal hemorrhage or cyst formationVariable delay in onset of menses and confusion regarding possibility of ectopic pregnancy: acute abdomen.
Ovary with hemorrhagic corpus luteum cystHemorrhagic corpus luteum with spider web like contentsHemorrhagic cyst with blood clot.Hemorrhagic cyst with unusual appearance simulating a neoplasm. Sonogram from a patient with bilateral theca lutein cysts. The typical multilocular appearance is noted in the left ovary.
Ovarian Endometriomas demonstrating hypoechoic cystic structures with low amplitude uniformly distributed echotexture in the cavity of the cyst. Benign epithelial tumors of the ovary can reach massive proportions. The serous cystadenoma seen here fills a surgical pan and dwarfs the 4 cm ruler2.Here is a benign serous cystadenoma that demonstrates multiloculation.
Note that the inner surface is, for the most part, smooth, with only a solitary papillation at the upper right.3. Ultrasound imaging4. Histopathological section: With few papillary projections from the surface. 1.Cut open section of mucinous cystadenoma.2. Histological section showing tall epithelial lining with pale staining nuclei at the basal pole.3.
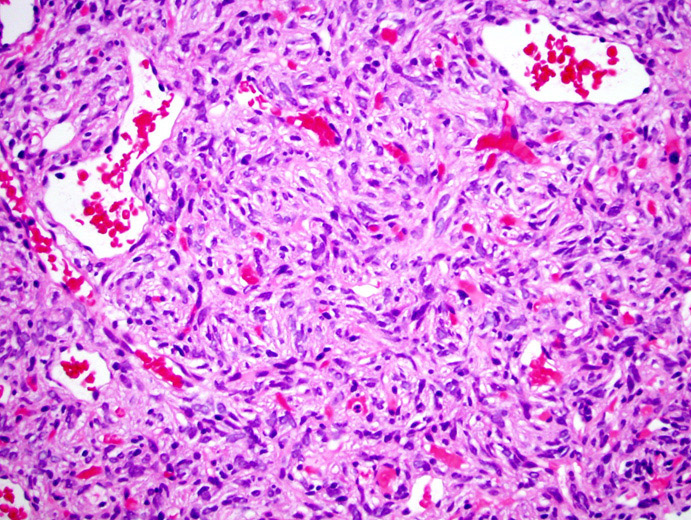
Variable echogenicity in the contents of an adnexal multilocular cyst. The photo below shows a well-developed tooth arising from the right side of the mural nodule ('Rokitansky nodule') that contains most of the solid teratomatous elements. The central portion of the nodule contains mostly cutaneous tissues (skin, sweat glands, and hair follicles), while the neural tissues extend into the wall toward the left. 1. Mature cystic teratoma with typical long hyperechogenic lines and bright prominent spots representing hair in fluid.2. Mature cystic teratoma with Rokitansky nodule or 'dermoid plug'(arrow) with posterior acoustic shadowing. grayish white and firmCut sectionMicroscopically – stellate or spindle shaped cells arranged in fusiform pattern. Hyalinisation is frequent.
The elongated fibroblastic tumor cells have spindle-shaped nuclei and may contain small amounts of lipid in their cytoplasm. Benign lesions can be managed by simple excision.t/t of malignant brenner tumours is unsettled, various forms of chemotherapy have been used with little success.Walthard cell rests are a benign cluster of epithelial cells most commonly found in the connective tissue of the Fallopian tubes, but also seen in the mesovarium, mesosalpinx and ovarian hilus. Solid, sharply circumscribed and pale yellow-tan in colour.
90% are unilateral (arising in one ovary, the other is unaffected). The tumours can vary in size from less than 1 centimetre (0.39 in) to 30 centimetres (12 in). Borderline and malignant Brenner tumours are possible but each are rare. Hyperplastic fibromatous matrix interspersed with nests of epitheloid cellsOn high magnification, they exhibit characteristic coffee bean nuclei (clearly visible in image). On low magnification, they resemble urothelial cell nests. Contralateral ovary may harbour macroscopically undetectable gonadoblastoma.Associated with dysgerminomas in 50%cases and with malignant germ cell tumours in an additional 10% cases.
Using these rules the reported sensitivity was 95%, specificity 91%, positivelikelihood ratio of 10.37 and negative likelihood ratio of 0.06. The morphology index (MI) presently used in the University of Kentucky Ovarian Cancer Screening Trial was published initially by Ueland and colleagues and is illustrated in Figure 49.3. Both morphologic complexity and tumor volume, as calculated by the prolate ellipsoid formula, were related directly to the risk of malignancyMorphologic abnormalities were easy to categorize, and interobserver variation was minimal. Risk of malignancy varied from 0.3% in ovarian tumors with a MI of =8. Using a MI =5 as indicative of malignancy, the following statistical parameters were observed: sensitivity 0.981, specificity 0.808, PPV 0.409, and NPV 0.997. Therefore, morphologic indexing is a relatively accurate and cost-effective method to predict risk of malignancy in an ovarian tumor.
Wenever possible conservative or minimally invasive surgery is preferred to preserve endocrine and reproductive function. BOTs form a separate entity within the group of ovarian tumours. BOTs can be divided according to their epithelialcharacteristics as serous (50%),mucinous (46%),and mixed, endometrioid, clear cell, or Brennertumors (3.9%). Serous BOTs are bilateral in 30%of patients and can be associated with extraovarian lesions (so-called implants) in 35%.
Theseimplants can be invasive or noninvasive depending on their microscopic appearance, which willin turn influence therapeutic options. MucinousBOTs are classified as intestinal (85%) or endocervical/Mullerian type (15%) depending on thenature of the epithelial lining. They can be associated with pseudomyxoma peritonei (10%), necessitating a thorough investigation of the GI tract with special attention to the appendix because thiscan be the primary tumor origin.Presenting symptoms of borderline ovarian tumorsBorderline tumors, as with other ovarian tumors, are difficult to detect clinically until they are advanced in size or stage. In one study, the most common presenting symptoms were abdominal pain, increasing girth or abdominal distention, and abdominal mass. Approximately 23% of patients were asymptomatic.
Without comprehensive surgical staging, the prognosis for an individual patient is difficult to predict.Many clinicians group stages II-IV together for prognostic consideration.Important component is description of the type of implants, as these have significant prognostic value.Preoperatively, borderline tumors are often presumed to be either benign or malignant ovarian masses; however, as with other ovarian masses, staging is performed surgically. Many sources recommend complete staging if a borderline tumor is found.
Current guidelines include biopsy specimens of the pelvic peritoneum (cul-de-sac, pelvic wall, and bladder peritoneum), abdominal peritoneum (paracolic gutters and diaphragmatic surfaces), omentum, intestinal serosa and mesentery, and retroperitoneal lymph nodes (pelvic and para-aortic). Borderline tumors are correctly diagnosed 58-86% of the time by frozen section, depending on the experience of the pathologist and the site of the operation (e.g.
Tertiary care vs community hospital). Postoperative treatment for any stage is controversial; therefore, recommending reoperation for surgical staging alone is difficult.3, 2 This being said, adequate staging is essential for determining the prognosis. Patients with stage I disease confirmed by comprehensive staging have a recurrence rate of approximately 15%.
The 5-year survival rate for such patients approaches 100%. However, the 10-year survival rate is 90-95%, depending on histologic findings.In patients with stage II-IV disease, the prognosis is different; an increased stage is associated with a worse prognosis and only age at diagnosis and the presence of invasive implants are shown to influence prognosis.In reported series, women who had serous tumors with noninvasive peritoneal implants demonstrated a mean 20% recurrence rate and a mean 7% death rate. In patients with recurrence, a median time to diagnosis of 3.1 years was reported if the recurrence was of the borderline type. In patients whose recurrence was invasive carcinoma, the median time to diagnosis was 8.3 years. It is believed that the former was a recurrence but that the latter was probably a new primary tumor. The cancer antigen 125 (CA-125) level was normal in 65% of the recurring cases (see the section Biomarkers and DNA Cytometry). Death was noted only when invasive carcinoma was noted in the recurrence.In patients with serous borderline tumors with invasive implants, the relapse rate was 31-45%, according to a study by Gershenson et al.4 The median time from diagnosis to recurrence was 24 months, although the time to progression of disease was significantly longer in patients who had no macroscopic disease remaining at the time of initial operation.4 Additionally, patients who received postoperative platinum-based chemotherapy had a significantly worse progression-free survival rate.
However, the authors of this study believed that this finding might have been due to selection bias.Gershenson and colleagues' research indicated that the following factors had no effect on progression-free survival:AgeStageType of surgeryPostoperative treatmentCoexistence with noninvasive implantsNumber of invasive implantsNo statistically significant differences are found in survival between mucinous and serous tumors. Mucinous tumors are most often stage I at time of diagnosis, and it is quite unusual to find extraovarian disease in tumors of mucinous origin. Preoperative transvaginal color Doppler ultrasonography has been used to assess the possibility of malignancy in ovarian masses. The rate of detection of intratumoral blood flow in borderline tumors (90%) is similar to that of malignant neoplasms (92%). The resistance and pulsatility indexes are also significantly reduced in carcinoma and borderline ovarian tumors compared with those of benign tumors.Although ultrasonography is useful in identifying the mass, this medium is not currently able to predict the final pathology of the tumor.
It is neither sensitive nor specific enough to be used as a screening tool in the normal populations. Computed tomography (CT) scanning should be considered preoperatively to identify possible foci of metastasis. CT scanning can also be useful when following the patient in the future. Again, as with ultrasonography, there are no distinguishing characteristics that clearly identify a borderline ovarian tumor. CA-125 levels are not shown to aid in the diagnosis or follow-up care of patients with borderline tumors. However, preoperatively, it can be useful in counseling the patient as to what to expect in the operating room.At present there is little evidence to supportanalysis of serum tumor markers in routine follow-up of patients with borderline ovarian tumors.
Surgical removal of BOTs is the cornerstone inthe management of BOTs, but a lot of debate existson the extent of the staging procedure and the surgical approach. Lately, the use of laparoscopy andconservative surgery, which is defined as surgerywith complete staging but withpreservation of theuterus and at least part of one ovary (Fig 1), is gaining popularity.
However, the question arises aboutwhether this management is appropriate or whetherwe should be more cautious. The accepted initial treatment of borderline ovarian tumors is surgical removal of the tumor and the performance of biopsies. However, the postoperative management protocol is far from clear. To date, no medical therapy has been shown to clearly improve outcomes.No consensus has been reached concerning treatment of patients with stage II-IV disease.
Although these women still have high 5-year survival rates compared with their counterparts with true malignant ovarian cancer, an increased stage is associated with a worse prognosis. However, stage (II vs III vs IV), type of surgery, postoperative treatment, postoperative platinum-based chemotherapy, and even the number of noninvasive implants have no effect on progression-free survival. Only age at diagnosis and the presence of invasive implants are shown to influence prognosis. Given the excellent prognosis for borderline ovarian tumors, hysterectomy and contralateral oophorectomy are not necessary (if the ovary appears normal) if the patient wishes to preserve fertility. If the patient is beyond childbearing age, then hysterectomy is a reasonable option. Removal of a normal, contralateral ovary should be based on existing data regarding ovarian physiology.3When a complex ovarian mass is discovered, surgery is often, if not always, indicated.
Complete excision of the disease must be achieved if at all possible. Comprehensive staging should be a part of every operation. Although stage may or may not affect future treatment, it is of significant prognostic value and therefore is of value to the clinician and to the patient.In one study, 77% of patients with invasive peritoneal implants also had noninvasive implants. Comprehensive debulking and staging decreases the chance of a sampling error that could result in an inaccurate diagnosis and prognosis.In most instances, surgery is curative for patients with confirmed stage I disease. If the tumor is unilateral and adjacent to normal tissue, unilateral cystectomy can be performed; however, inspection of the capsule for signs of rupture should be performed before resection. If no normal adjacent tissue is present, oophorectomy or salpingo-oophorectomy should be performed.
Benign Ovarian Tumours
If the contralateral ovary is normal in appearance, a biopsy should not be performed on the adjacent ovary because of the risk of ovarian failure (if fertility is an issue).Owing to the high association between surface proliferations and peritoneal implants, exploration of the peritoneum should be extensive and thorough. If possible, carefully evaluate and remove the implants. The type of implant (ie, invasive, noninvasive) should be noted by pathology, as it has significant prognostic value.Contraindications to surgery include medical reasons (ie, the patient is too great a surgical risk secondary to other medical problems) or patient refusal.
Otherwise, the masses should be surgically removed. Various chemotherapy regimens have been used, but evidence is insufficient to determine exactly which therapy is indicated for borderline ovarian tumors. Many authors have used platinum-based agents, but with varying results. Some authors recommend platinum-based therapy for patients with invasive peritoneal implants because of their worse prognosis. Standard chemotherapy regimens for invasive ovarian cancer are used if any medical therapy is given. In patients without metastatic disease, chemotherapy is not indicated.An important area of research is postoperative chemotherapy.
Little advantage has been reported after postoperative chemotherapy, but the number of patients studied has been small and the chemotherapeutic regimens used have been varied. The general consensus is that borderline tumors with noninvasive implants do not require any further therapy and should be observed. However, the benefit of treating tumors with invasive implants has been discussed. To date, no randomized data show a benefit.
Benign ovarian tumours. 1. SRAVANTHI DR.